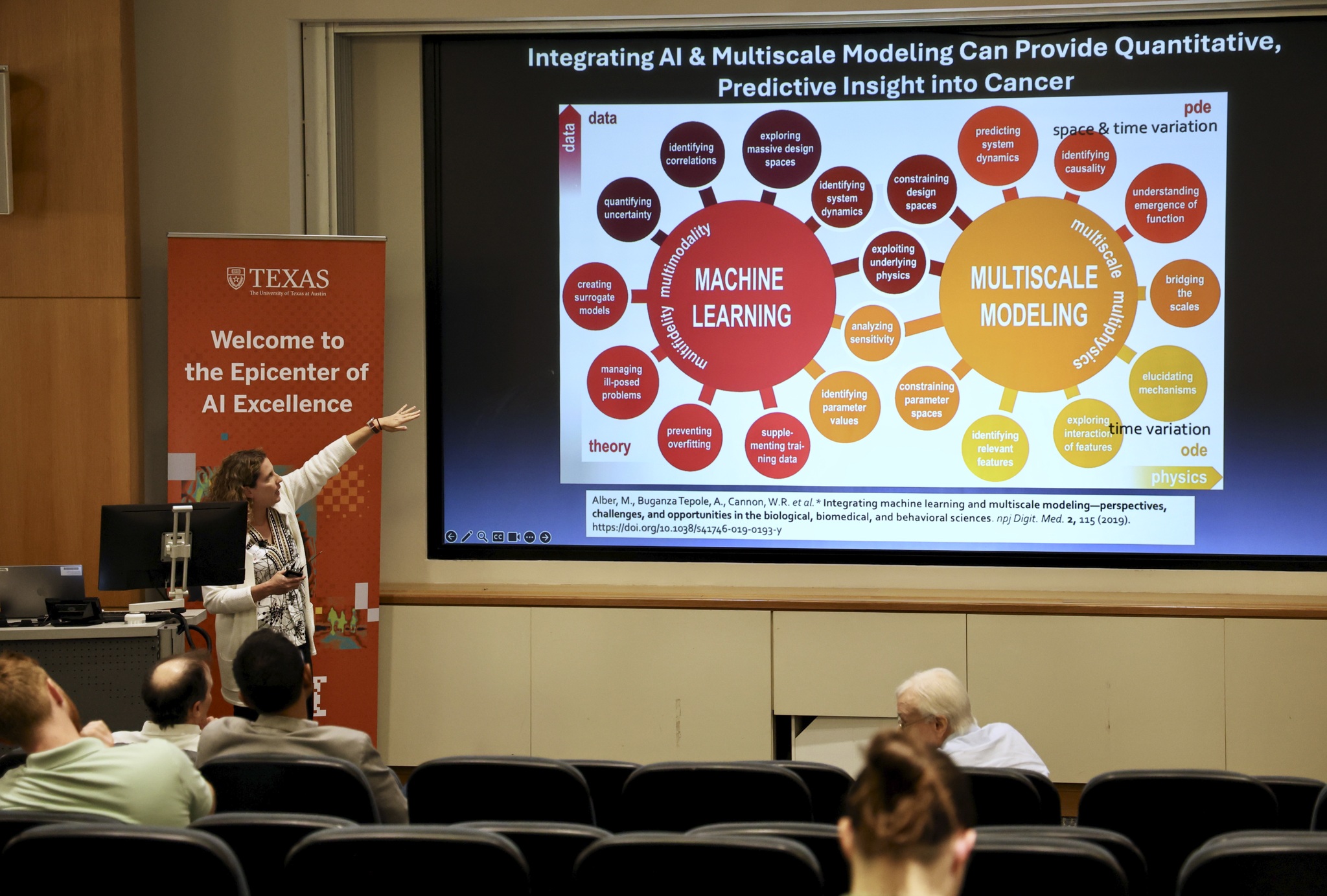
What does the hospital of the future look like? Recent advances in Artificial Intelligence (AI), deep learning, and digital twin technologies that predict tumor growth, analyze drug activity, and serve as diagnostic tools make this ‘tomorrowland’ look more possible than ever before.
'Realistic Goals for AI in Oncology,' a half-day workshop held on September 16, hosted by Tom Yankeelov, director for the Center of Computational Oncology at the Oden Institute for Computational Engineering and Sciences, considered just that. The workshop, part of The University of Texas at Austin's Year of AI, featured experts at the forefront of bridging medicine with Artificial Intelligence, speakers and attendees bridged the gap between our wildest dreams for futuristic cancer diagnosis with scientifically, ethically, and economically sound principles for the application of AI in oncological healthcare. “The goal of this workshop is an attempt to strip away some of that hype to identify problems in oncology for which AI is well-suited to practically solve,” shared Yankeelov, as attendees and speakers filtered into the Peter O'Donnell Building’s Avaya Auditorium.